Myocarditis is an inflammatory disease of the heart muscle, whilst pericarditis is an inflammatory disease of the lining of the heart muscle. They are rare conditions, most commonly associated with viral infections (including SARS-CoV-2) but can also be triggered by other factors such as medications and autoimmune conditions.
Globally, an increased number of cases above an expected population rate of myocarditis and pericarditis have been reported in individuals who have received COVID-19 vaccines, with the highest rates occurring following administration of COVID-19 mRNA vaccines (eg. Comirnaty (Pfizer) and Spikevax (Moderna)).
Information specific to myocarditis and pericarditis can be found via the below buttons. In addition, frequently asked questions relating to vaccination are also addressed.
How is myocarditis following COVID-19 vaccination triggered?
The exact mechanism behind cardiac inflammation temporally associated with COVID-19 vaccines is currently being investigated. Clinical causes from international and local surveillance data suggest an immune-mediated or hypersensitivity trigger. There are ongoing studies examining the role of the SARS-CoV-2 spike protein, impact of certain cardiac biomarkers and genetic predispositions to this adverse event of special interest (AESI).
Who is at risk of myocarditis?
Myocarditis from any cause, occurs more commonly in males than females. It is also more likely to affect younger adults.
Reported rates of myocarditis occurring following administration of COVID-19 vaccines vary; however, they are above expected background rates for both sexes. The peak risk group for COVID-19 vaccine related myocarditis is young adult males aged 16-17 years, with a smaller increased risk for males aged between 12-24 years.
International and local vaccine safety surveillance data have found that it is more commonly associated with administration of a second dose of COVID-19 mRNA vaccine. Myocarditis following other COVID-19 vaccines, third doses or booster doses have also been identified, although reported cases have occurred at lower rates than those identified following either dose of a primary course.
Although myocarditis AESI has been associated with all of the COVID-19 vaccines used in Australia, there is a higher risk of myocarditis following administration of COVID-19 mRNA vaccines compared to non-mRNA vaccines. Surveillance data from multiple countries have also demonstrated a greater risk with Spikevax (Moderna) compared to Comirnaty (Pfizer).
Are children more likely to experience myocarditis following COVID-19 vaccination?
Available safety data from local and international sources suggest there is a significantly lower risk of children developing myocarditis following vaccination. Thus far, data shows that the risk of COVID-19 vaccine myocarditis decreases as age decreases.
ATAGI recommends an interval of 8 weeks between vaccine doses in a primary course for age-eligible children (≤ 11 years) for maximum efficacy and safety. This extended interval is based on international data suggesting a longer time interval between dose 1 and 2 may reduce the risk of myocarditis. This extended interval also allows more time to observe international vaccine safety data and identify any signals for rare adverse events.
Very few cases of myocarditis in children <6 years of age have been reported in available worldwide surveillance data to date.
For more information on COVID-19 vaccination in individuals < 18 years please refer to COVID-19 vaccination in children and adolescents.
Pre-existing cardiac conditions and COVID-19 vaccination
Individuals with the following cardiac conditions can safely receive COVID-19 vaccines without the need for additional monitoring or precautions:
- coronary artery disease
- myocardial infarction
- stable heart failure
- arrhythmias
- rheumatic fever
- rheumatic heart disease
- kawasaki disease
- most congenital heart disease
- those with implanted cardiac devices
- congenital heart disease
- cardiac transplant
- cardiomyopathy.
Those with a history of the following conditions can also receive COVID-19 vaccines; however should consult their treating specialist to determine the appropriate timing for vaccination:
- recent (within 3 months) or current inflammatory cardiac conditions (including myocarditis, pericarditis and endocarditis)
- acute rheumatic fever or acute rheumatic heart disease
- acute decompensated heart failure.
Patients with ongoing cardiac inflammation should have vaccination deferred. In some instances, vaccination with Vaxzevria (AstraZeneca) or Nuvaxovid (Novavax) may be considered due to the lower associated risk of developing myocarditis.
What are the symptoms of myocarditis?
Myocarditis presents similarly to pericarditis, with a range of symptoms including:
- chest pain, pressure or discomfort
- pain with breathing (pleuritic chest pain)
- shortness of breath
- palpitations
- syncope (faint)
- other non-specific symptoms such as fatigue, dizziness, abdominal pain.
In individuals who have received COVID-19 vaccines, symptoms of myocarditis have most commonly been reported within 2-7 days of second dose vaccination.
How is myocarditis after COVID-19 vaccination diagnosed and investigated?
If there is suspicion of myocarditis, particularly in the first week following vaccination, timely medical review is important. Those who appear unwell should be referred to an emergency department for examination and the following primary investigations:
- blood tests for cardiac biomarkers, such as troponin
- electrocardiogram (ECG).
Other tests should be considered if the patient is unwell or the tests above are abnormal:
- chest X-ray (CXR)
- other tests related to investigating differential diagnoses such as inflammatory markers (C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)
- bedside or formal ultrasound/echo
- cardiac MRI.
Consistent findings of myocarditis may include elevated troponin, ECG changes (ST or T-wave abnormalities, premature atrial or ventricular complexes) as well as abnormal echocardiogram or cardiac MRI.
Individuals who are investigated for myocarditis following vaccination should avoid high-intensity exercise until symptoms have resolved is recommended.
Cardiologist advice and followup is strongly recommended.
How is myocarditis after COVID-19 vaccination treated?
Current data shows that most cases of myocarditis following COVID-19 vaccination have mild symptoms and recover well. Information on long term sequelae is not yet available.
Treatment of these conditions is managed by a cardiologist and include in-patient supportive therapies. In the rare severe or complicated cases, specific management for arrythmias, decreased cardiac function or congestive cardiac failure with pharmacological agents such as ACE-inhibitors and beta-blockers or mechanical support may be necessary.
I have specific questions around my risk of myocarditis following COVID-19 vaccination. Help!
Although uncommon, myocarditis is most often seen after COVID-19 mRNA vaccines. Please refer to our specific FAQs on COVID-19 mRNA vaccines for further information. This includes answers on:
- impact of dose intervals between 1st and 2nd doses of vaccine
- risk of developing myocarditis from COVID-19 disease vs the vaccine
- exercise after COVID-19 vaccination
- impacts of medications and drugs such as clozapine, stimulants, amphetamines on developing myocarditis.
What are the implications for future doses (including third and booster doses)?
For individuals where the cause of inflammation is attributed to COVID-19 vaccination, a report to SAEFVIC is indicated and a referral to a cardiologist and/or specialist immunisation service (eg. VicSIS) is recommended.
Please refer to the below algorithm for recommendations relating to further doses of COVID-19 vaccines in patients who have been diagnosed with myocarditis following vaccination.
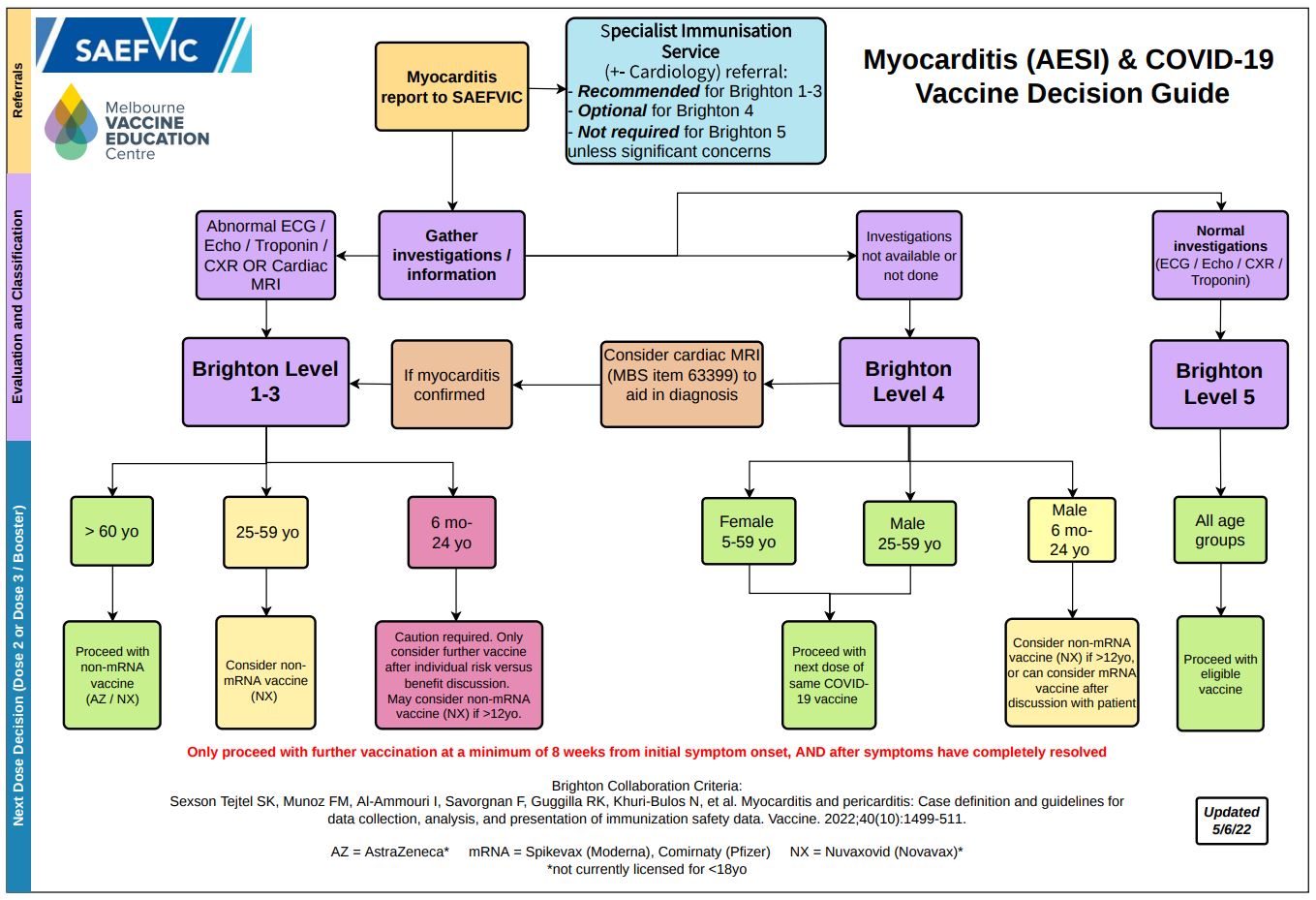 *Brighton Level refers to Brighton Collaboration criteria for classifying myocarditis
*Brighton Level refers to Brighton Collaboration criteria for classifying myocarditis
PDF version of the above diagram available here.ATAGI currently recommends that individuals diagnosed with myocarditis following vaccination defer any further doses and are referred to a specialist immunisation clinic.
What is the risk/benefit ratio for vaccination for the young adult age group?
It is important to discuss your individual circumstances with a health care provider in order to make an informed decision.
The level of COVID-19 community transmission in Australia can change quickly. Factors to consider include age, potential for exposure to the virus (including in the workplace), high rates of global transmission, the emergence of new variants of the virus, as well as the potential for future changes to Australia’s border controls.
Whilst COVID-19 infection can sometimes result in myocarditis, its incidence following COVID-19 vaccination is comparatively extremely rare. Most individuals diagnosed with myocarditis following COVID-19 vaccination have responded well to treatment.
How is pericarditis following COVID-19 vaccination triggered?
The exact mechanism behind cardiac sac inflammation temporally associated with COVID-19 vaccination is currently being investigated. Clinical causes from international surveillance data suggest an immune-mediated or hypersensitivity trigger.
Who is at risk of pericarditis?
Pericarditis from any cause occurs in similar rates amongst males and females. It is also more likely to affect younger adults.
Reported rates of pericarditis occurring following administration of a COVID-19 vaccine vary; however, they are above expected background population rates. Available surveillance data suggests the risks for pericarditis after a mRNA vaccine are higher than non-mRNA vaccines.
International and local data indicate that pericarditis following COVID-19 vaccines is more common in the 18-39 year old age group for both males and females. Pericarditis following third doses or booster doses have also been identified in a small number of individuals. Reported cases have occurred at significantly lower rates than those identified following either dose of a primary course.
Are children more likely to experience pericarditis following COVID-19 vaccination?
Available safety data from local and international sources suggest there is a significantly lower risk of children developing pericarditis following COVID-19 vaccination.
ATAGI recommends an interval of 8 weeks between vaccine doses in a primary course for age-eligible children (≤ 11 years) for maximum efficacy and safety. This extended interval is based on international data suggesting a longer time interval between dose 1 and 2 may reduce the risk of myocarditis – which in principle may also extend to pericarditis. This extended interval also allows more time to observe international vaccine safety data and identify any signals for rare adverse events.
For more information on COVID-19 vaccination in individuals < 18 years please refer to COVID-19 vaccination in children and adolescents.
Pre-existing cardiac conditions and COVID-19 vaccination
Individuals with the following cardiac conditions can safely receive COVID-19 vaccines without the need for additional monitoring or precautions:
- coronary artery disease
- myocardial infarction
- stable heart failure
- arrhythmias
- rheumatic fever
- rheumatic heart disease
- kawasaki disease
- most congenital heart disease
- those with implanted cardiac devices
- congenital heart disease
- cardiac transplant
- cardiomyopathy.
Those with a history of the following conditions can also receive COVID-19 vaccines; however should consult their treating specialist to determine the appropriate timing for vaccination:
- recent (within 3 months) or current inflammatory cardiac conditions (including myocarditis, pericarditis and endocarditis)
- acute rheumatic fever or acute rheumatic heart disease
- acute decompensated heart failure.
Patients with ongoing cardiac inflammation should have vaccination deferred. In some instances, vaccination with Vaxzevria (AstraZeneca) or Nuvaxovid (Novavax) may be considered due to the lower associated risk of pericarditis.
What are the symptoms of pericarditis?
Pericarditis presents similarly to myocarditis, with a range of symptoms including:
- chest pain, pressure or discomfort
- pain with breathing (pleuritic chest pain)
- shortness of breath
- palpitations
- syncope (faint)
- other non-specific symptoms such as fatigue, dizziness, abdominal pain.
How is pericarditis after COVID-19 vaccination diagnosed and investigated?
If there is suspicion of either of these conditions, particularly in the first 2-3 weeks following vaccination, timely medical review is important. Those who appear unwell should be referred to an emergency department for the following investigations:
- blood tests for cardiac biomarkers, such as troponin
- electrocardiogram (ECG)
Other tests should be considered if the patient unwell or the tests above are abnormal:
- chest X-ray (CXR)
- other tests related to investigating differential diagnoses such as inflammatory markers (C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR)).
Consistent findings of pericarditis include a pericardial rub on auscultation, widespread ST-elevation or PR depression on ECG, as well as pericardial effusion on imaging.
Individuals who are investigated for pericarditis following vaccination should avoid high-intensity exercise until symptoms have resolved is recommended. Those experiencing ongoing symptoms should return for review in 1-2 days time. Cardiologist advice is recommended if clinical suspicion is high, regardless of normal investigations.
How is pericarditis after COVID-19 vaccination treated?
Current data shows that most cases of pericarditis following COVID-19 vaccination have mild symptoms and recover well.
In some scenarios, there have been reports of pericarditis causing prolonged and recurrent symptoms but with functionally normal investigations including cardiac imaging. Information on long term sequelae is still being collected.
Treatment of these conditions is managed by a cardiologist and include in-patient supportive therapies, often with anti-inflammatory medications or colchicine. In the rare severe or complicated cases, specific management for arrhythmias, decreased cardiac function or congestive cardiac failure with pharmacological agents such as ACE-inhibitors and beta-blockers or mechanical support may be necessary.
What are the implications for future doses (including third and booster doses)?
For individuals where the cause of inflammation is attributed to COVID-19 vaccination, a report to SAEFVIC is indicated and a referral to a cardiologist and/or specialist immunisation service (eg. VicSIS) is recommended.
Please refer to the below algorithm for recommendations relating to further doses of COVID-19 vaccines in patients who have been diagnosed with pericarditis following vaccination.
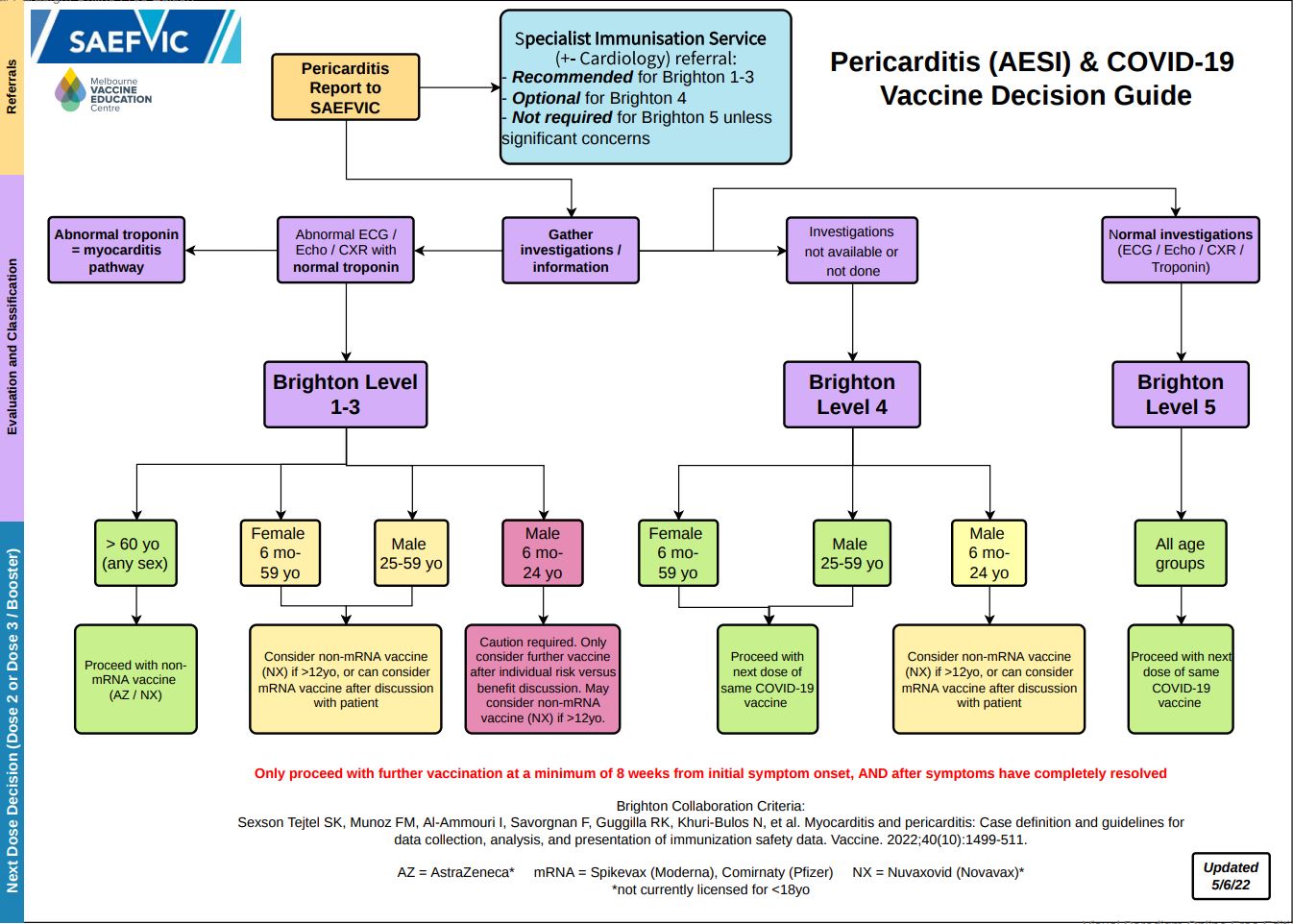 *Brighton Level refers to Brighton Collaboration criteria for classifying pericarditis
*Brighton Level refers to Brighton Collaboration criteria for classifying pericarditis
Access a pdf version of this guide here.In particular, the groups which are at lower risk (green in algorithm), could proceed with further doses of COVID-19 vaccination as per above suggested instructions.
What is the risk/benefit ratio for vaccination for the young adult age group?
It is important to discuss your individual circumstances with a health care provider in order to make an informed decision.
The level of COVID-19 community transmission in Australia can change quickly. Factors to consider include age, potential for exposure to the virus (including in the workplace), high rates of global transmission, the emergence of new variants of the virus, as well as the potential for future changes to Australia’s border controls.
Whilst COVID-19 infection can sometimes result in pericarditis, its incidence following COVID-19 vaccination is comparatively extremely rare. Most individuals diagnosed with pericarditis following COVID-19 vaccination have responded well to treatment.
I am taking certain medications that have myocarditis listed as an uncommon side effect. Am I at greater risk of developing myocarditis/pericarditis after COVID-19 vaccination?
Taking medications that have myocarditis listed as an uncommon side effect (e.g. antipsychotic drugs and biological chemotherapeutic agents) is not a contraindication to COVID-19 vaccination. Individuals taking these medications can be safely vaccinated in the community with no need for additional precautions or monitoring.
Are there impacts of other substances on the development of myocarditis/pericarditis after COVID-19 vaccines?
The use of recreational stimulants (particularly amphetamines) is discouraged especially in the week following vaccination to limit the potential for developing myocarditis/pericarditis.
Should exercise be limited after receiving COVID-19 vaccines to reduce the chance of myocarditis/pericarditis?
Exercise is not thought to increase the risk of developing myocarditis/pericarditis following COVID-19 vaccination. It is therefore not necessary to reduce or avoid exercise in the post-vacccination period.
However, if patients develop myocarditis/pericarditis post vaccination there is a concern that exercise may be pro-arrhythmic (eg. will exacerbate) the condition.
As myocarditis/pericarditis following COVID-19 vaccination is thought to be immune mediated, would those with pre-existing autoimmune diseases be at an increased risk compared to the general public?
Myocarditis/pericarditis following COVID-19 vaccination appears to be idiosyncratic at this stage, with no clear risk factors. Thus, there is no indication of increased risk in those with underlying autoimmune disease.
Resources
Investigation, management and treatment of myocarditis/pericarditis
- HealthPathways Myocarditis and Pericarditis after mRNA COVID-19 Vaccines (login required)
- Paediatric Research in Emergency Departments International Collaborative: Chest pain guideline
Guidelines on Myocarditis/Pericarditis
- COVID-19 vaccination – Guidance on myocarditis ad pericarditis after COVID-19 vaccines
- CDC Clinical Considerations: Myocarditis and Pericarditis after Receipt of mRNA COVID-19 Vaccines Among Adolescents and Young Adults
- COVID-19 subcommittee of the WHO Global Advisory Committee on Vaccine Safety (GACVS) reviews cases of mild myocarditis reported with COVID-19 mRNA vaccines
- Brighton Collaboration: Myocarditis/Pericarditis Case Definition
MVEC resources on COVID-19 vaccines and myocarditis/pericarditis
Authors: Rachael McGuire (MVEC Education Nurse Coordinator), Francesca Machingaifa (MVEC Education Nurse Coordinator), Daryl Cheng (MVEC Medical Lead) and Nigel Crawford (Director SAEFVIC, Murdoch Children’s Research Institute)
Reviewed by: Daryl Cheng (MVEC Medical Lead) and Julia Smith (Immunisation Fellow, Royal Children’s Hospital)
Date: October 27, 2022
Materials in this section are updated as new information and vaccines become available. The Melbourne Vaccine Education Centre (MVEC) staff regularly reviews materials for accuracy.
You should not consider the information in this site to be specific, professional medical advice for your personal health or for your family’s personal health. For medical concerns, including decisions about vaccinations, medications and other treatments, you should always consult a healthcare professional.