Most vaccines available for use in Australia are administered via intramuscular or subcutaneous route, with several being administered intradermally or orally. Administering vaccines via the recommended route and using correct technique is of paramount importance to ensure optimal immune response, minimise side effects and reduce the risk of injury to the patient.
Routes of administration
Intramuscular
Intramuscular vaccines are administered into the muscle layer of tissue at a 90° angle. Muscle contains a vast amount of blood vessels resulting in increased blood supply which enables the vaccine to disperse easily. In addition, muscles contain dendritic (antigen-presenting) immune cells that initiate a long-lasting immune response. Intramuscular vaccines tend to have fewer side-effects other than redness and pain at the injection site, which are usually mild and short lived.
Subcutaneous
Subcutaneous vaccines are administered into the subcutaneous, or fatty layer beneath the skin at a 45° angle. Vaccines designed for subcutaneous administration are absorbed at a slower and more constant rate as there is less blood supply in subcutaneous tissue than muscle.
Intradermal
Intradermal vaccines are administered into the outer layers of skin, between the epidermis and the dermis at a 5-15° angle. The epidermal and dermal layers contain many different cells including the antigen-presenting cells (APC’s) that are thought to play a significant role in mediating an efficient and protective immune response to specific vaccines. The 3 main APC’s are macrophages, dendritic cells and B cells. APC’s present specific antigens to particular cells in the immune system that are responsible in eliciting an immune mediated response that in turn creates memory cells and antibodies.
Intradermal vaccination is a unique method of vaccine delivery which requires specific training to ensure vaccine safety and efficacy.
Oral
Oral vaccines activate immune cells in the mucousal membranes lining the gastrointestinal tract which is beneficial in protecting against diseases that affect the gut.
Depending on the vaccine, oral vaccines can come in either tablet or liquid formulation. Liquid vaccines recommended for oral administration should never be injected. Oral vaccines available in tablet form should not be chewed or broken.
Please note, if an infant receiving an oral vaccine spits out a small amount of the dose of vaccine it is still considered a valid dose and doesn’t need repeating. If they spit out most of the dose of vaccine within minutes of receiving it, a repeat dose should be administered at the same visit.
Injectable vaccines
Intramuscular and subcutaneous injection
Recommended site for injection in infants < 12 months of age
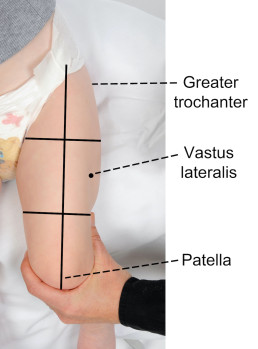
The recommended injection site is the middle third of the vastus lateralis (anterolateral thigh).
To locate the correct anatomical site for injection:
- ensure the infant’s leg is completely exposed
- locate the upper and lower anatomical landmarks- greater trochanter of femur and patella
- draw an imaginary line between the 2 landmarks down the front of the thigh
- then imagine the thigh is divided into thirds
- the correct injection site is located in the middle third and on the outer aspect of the imaginary line (see images below).
Where only two vaccines are scheduled it is recommended to give one vaccine into each thigh. If more than two vaccines are recommended at the one visit, two vaccines may be given into each thigh ensuring they are separated by 2.5 cm (refer to images below). When administering more than one vaccine into the same thigh, it is important to consider the reactogenicity of each vaccine. Those that are considered more reactogenic should be in different thighs where possible. For example, meningococcal B (Bexsero®) is frequently associated with increased local site reactions.
In some circumstances where the thigh cannot be used (e.g. congenital limb malformations, active eczema or hip brace placement) the deltoid may be used (refer to the recommended site for injection in children ≥ 12 months for guidance).

Recommended site for injection in children ≥ 12 months of age, adolescents and adults
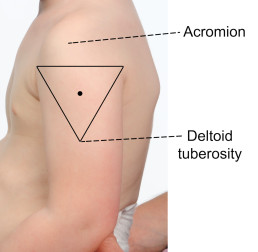
The recommended injection site is the deltoid (upper arm).
To locate the correct anatomical site for injection:
- expose the arm completely from the top of the shoulder to the elbow; remove shirt or clothing if needed
- locate the upper and lower anatomical landmarks- acromion (shoulder tip) and the muscle insertion of the deltoid (deltoid tuberosity)
- draw an imaginary inverted triangle below the shoulder tip, using the identified landmarks (see images below)
- the site for injection is halfway between the acromion and the deltoid tuberosity, in the middle of the deltoid muscle (triangle).
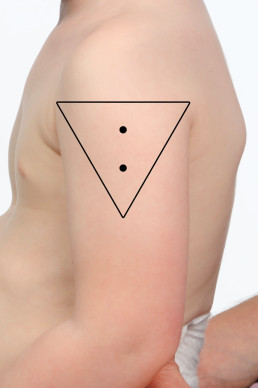
Two or more vaccines may be given into the same deltoid ensuring they are separated by 2.5 cm (refer to images below). When administering more than one vaccine into the same deltoid, it is important to consider the reactogenicity of each vaccine. Those that are considered more reactogenic should be in different deltoids where possible. For example, meningococcal B (Bexsero®) and pneumococcal polysaccharide (Pneumovax® 23) are frequently associated with increased local site reactions.
Utilising the anterolateral thigh may also be required in this age group (e.g. congenital limb malformations, history of auxillary clearance, active eczema or insufficient spacing available). In these circumstances, there is a preference for administering the least reactogenic vaccines via this site (refer to the recommended site for injection in children ≤ 12 months for guidance).
Intradermal injection
Recommended sites for intradermal injection in any age
The recommended sites for intradermal administration are the volar (inner) surface of the mid-forearm or over the deltoid region over where the deltoid muscle inserts into the humerus.
The deltoid region on the left arm is specifically recommended for BCG administration in any age groups as administration at this site minimises the risk of keloid scarring.
Which vaccines can be given intradermally?
Examples of vaccines given by the ID route include BCG and hepatitis B (for non-responders). Mantoux and Q Fever tests are also performed intradermally.
Hepatitis B vaccine is usually given by the IM route however there is a small percentage of the population who do not mount a protective immune response to the IM course of hepatitis B vaccines. If they have been deemed by their provider as a non-responder the intradermal route is considered as an alternative [refer to MVEC: Hepatitis B for more information].
WordPress Tables PluginVaccine Dose Recommended site BCG (tuberculosis) < 12 months 0.05ml
≥ 12 months 0.1mlLeft upper arm over the region where the deltoid muscle inserts into the humerus§ Engerix®-B Adult (hepatitis B)¥ 0.25ml (20mcg/1.0ml) per dose Left upper arm over the deltoid region Jynneos® (MPX) 0.1ml Left upper arm over the deltoid region or the volar surface of the mid-forearm Tuberculin skin test (TST/Mantoux) 0.1ml Volar surface of mid-forearm Q-Vax skin test (Q fever test) 0.1ml of diluted Q-Vax skin test Volar surface of mid-forearm §This is the recommended site to minimise the risk of keloid formation
¥Refer to MVEC: Hepatitis B for more information on the management of non-respondersIntradermal vaccination technique
- Use a short (10mm) 26-27 gauge needle with a short bevel and a 1ml insulin syringe
- Wear protective eye wear when administering BCG vaccine as eye splashes can ulcerate
- Identify the correct injection site (see Table 1 above)
- Stretch the skin between a finger and your thumb
- Insert the bevel into the dermis with the bevel facing upwards, to a distance of approx. 2mm. The bevel should be visible through the epidermis
You should feel resistance as you inject, if you don’t, the needle may be in subcutaneous tissue. If the injection is not intradermal, withdraw the needle and repeat at a new site. When given correctly, an intradermal injection should raise a blanched bleb.
Preparing the site for injection
The skin at the injection site should be visibly clean prior to administering a vaccine. The swabbing of clean skin before giving an injection is not necessary. If the skin is visibly dirty, clean the site with alcohol wash/single use alcohol swab and allow the site to dry completely before administering the injection. If active/infected eczema is present at the recommended site, consider an alternate site to minimise the risk of injection site abscess. If there is no alternate site suitable, consider cleaning the site with an alcohol based wash/single use alcohol swab and allowing the site to dry completely before injecting.
Recommended needle size, length and angle for administering vaccines
| Age or size of the patient | Needle type | Angle of needle insertion |
| Infant, child or adult for IM injection | 22 – 25 gauge, 25mm in length | |
| Preterm infant or very small infant for IM injection | 23 – 25 gauge, 16mm in length | |
| Very large/obese patient for IM injection | 22 – 25 gauge, 38mm in length | |
| Subcutaneous injection in all patients | 25 – 27 gauge, 16mm in length | |
| Intradermal injection in all patients | 26 – 27 gauge, 10mm in length | 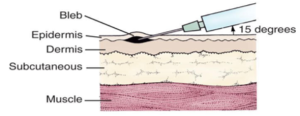 |
* Table adapted from the Australian Immunisation Handbook
Positioning for vaccination
Infants and younger children
It is important that children remain still during a vaccination to ensure that the vaccine can be administered into the correct anatomical site, as well as reduce the risk of any unintended injury (eg. needle stick injury). It is important to involve both the child and parent/guardian in discussions when deciding if a child can sit independently or requires support. When positioning a child for vaccination it is important to ensure that they are comfortable and the mobile joints of the limb receiving the vaccine are stable. The immunisation provider must be able to adequately visualise the anatomical landmarks and correct site for injection (deltoid or anterolateral thigh).
Infants can be held in the cuddle position or on their parents lap facing the provider, with the parent/guardian holding their arms securely and their thighs completely exposed. Younger children can be held in the cuddle or straddle positions with their upper arm completely exposed as demonstrated in the clip below.
For infants receiving oral vaccines, it is recommended they are positioned in such a way that the vaccine can be administered via gentle squeezing of the vaccine tube into their inner cheek, such as a feeding position.
Older children, adolescents and adults
It is recommended that older children, adolescents and adults sit in a straight-backed chair with their feet on the floor for vaccine administration. Providers should encourage the vaccine recipient to relax their forearms and rest their hands on their upper thighs, keeping their arms flexed at the elbow to assist in relaxing the deltoid muscle.
Vaccine recipients who are prone to vasovagal responses (fainting) should be vaccinated lying down to prevent unintended injury due to a fall.
Resources
Authors: Mel Addison (SAEFVIC Research Nurse, Murdoch Children’s Research Institute) and Rachael McGuire (SAEFVIC Research Nurse, Murdoch Children’s Research Institute)
Reviewed by: Francesca Machingaifa (MVEC Education Nurse Coordinator) and Rachael McGuire (MVEC Education Nurse Coordinator)
Date: July 6, 2023
Materials in this section are updated as new information and vaccines become available. The Melbourne Vaccine Education Centre (MVEC) staff regularly reviews materials for accuracy.
You should not consider the information in this site to be specific, professional medical advice for your personal health or for your family’s personal health. For medical concerns, including decisions about vaccinations, medications and other treatments, you should always consult a healthcare professional.