结核病
什么是流行性感冒?
结核病(简称TB)是因为感染了结核杆菌而引发。在较罕见的病例中,结核病也可能是因为感染牛分枝杆菌或非洲分枝杆菌而导致。
结核病可划分为活动性疾病(受感染的患者出现相关症状,并具有传染力)或潜伏性感染(细菌处于休眠状态,受感染的患者不出现相关症状,也没有传染力)。由于严重疾病、滥用毒品或酗酒、或者随着年龄的增长,潜伏性结核感染可能会因为某种病况或接受免疫抑制疗法而使免疫系统弱化,进而发展为活动性结核病。
流感症状
在澳大利亚,大约60%的结核病例属于肺结核。常见症状包括慢性咳嗽,同时可能伴随咯血以及发烧、盗汗、体重下降和不适(一般感觉不适)。
在某些情况下,感染会出现在脑部、骨骼、肾脏或淋巴结中。结核性脑膜炎(脑部感染)和结核性败血症(血液感染)被认为是结核病的最严重表现形式。
大部分感染结核病的人是无症状的。感染结核病的人中,有10%会在其人生的某个时候发展为临床疾病。
结核病是如何传播的?
肺结核患者在咳嗽或打喷嚏时,其受感染的飞沫会以气溶胶传播的方式传染给其他人。感染结核病的患者,如果其肺部或喉部不受影响,则通常不会传播这种疾病。不过,肾结核病患者的尿液具有传染性。在牛分枝杆菌盛行的国家(在澳大利亚不盛行),这种细菌也可以通过摄入未经巴氏法高温杀菌的牛奶而传播。
在经过主动治疗后14天以及痰液样本检测为阴性之前,通常认为此时患者具有传染能力。受到活动性感染后,该细菌会在瘢痕组织中保持休眠状态(无感染性),并可能在之后才被重新激活(甚至在几十年之后)。被重新激活后,细菌就再次具有传播能力。
流行病学
澳大利亚是世界上结核病感染率最低的国家之一,每10万人中只有不到7人会受到感染。居住在北领地和昆士兰州远北地区的原住民及托雷斯海峡岛民受这种疾病的影响非常大,远高于同地区的非土著居民,也远高于居住在其他州的原住民及托雷斯海峡岛民。
从全球来看,估计全球大约有四分之一的人口感染了结核病,并且每年导致一百五十万人死亡。孟加拉、中国、印度、印尼、尼日利亚、巴基斯坦、菲律宾和南非的感染发病率最高,全世界将近一半的结核病例发生在这些地区。
5岁以下儿童、老年人、免疫力低下(由于健康状况或免疫抑制治疗)人群以及生活条件较差群体的感染率最高。
预防措施
在结核病盛行的国家,接种卡介苗(BCG)疫苗能有效地减少结核性脑膜炎的发病率以及5岁以下儿童的死亡率。在该疾病发病率较低的发达国家,例如澳大利亚,不建议作为常规疫苗进行接种。在澳大利亚,我们建议以下人群接种该疫苗:
- 在昆士兰州原住民及托雷斯海峡岛民社区居住的5岁以下儿童
- 居住在昆士兰州的原住民及托雷斯海峡岛民新生婴儿
- 5岁以下儿童到结核病盛行地区进行国际旅行
旅行 至结核病高发地区的人士,最好是在出发前4到6周接种卡介苗疫苗
结核菌素皮肤试验
在接种卡介苗疫苗前,建议按具体情况进行结核菌素皮肤试验或芒图试验,以判断某个人身上是否已经具有一定程度的结核病免疫能力。该试验是指在皮内注射结核菌素纯蛋白衍生物(PPD)。
如果受试对象之前曾接种过卡介苗疫苗,或者之前曾感染结核病,则在48至72小时后就能观察到超敏反应。
需要注意的是,感染麻疹或接种含麻疹疫苗后的4至6个星期内,结核菌素皮肤试验的结果可能不可靠。
疫苗接种
卡介苗疫苗是通过皮内注射进行接种。只有经过皮内技术培训的医疗护理提供者方可提供卡介苗疫苗接种。
推荐的注射部位是左上臂三角肌插入肱骨的位置。在这个部位注射可最大程度地降低出现瘢痕疙瘩的风险。
- 对于年龄为12个月以下儿童,推荐剂量为0.05毫升。
- 对于年龄为12个月以上儿童,推荐剂量为0.1毫升。
其他注射型减毒活疫苗可以与卡介苗疫苗一起在同一天接种,或者间隔4个星期接种。卡介苗疫苗与口服型减毒活疫苗之间没有建议的接种间隔时间。
禁忌症与注意事项
卡介苗是减毒活疫苗,因此正接受免疫抑制治疗的人士或怀孕妇女忌用。
如果注射部位出现湿疹、皮炎或银屑病,则应推迟接种,直至皮肤经过治疗、症状得以消除后再接种。
免疫接种的副作用
和所有疫苗一样,在接种卡介苗疫苗后的几个星期内,也有一些常见和可预见的副作用,也可能会出现一些罕见的副作用。
常见和可预见的副作用包括:
- 在接种疫苗后的几个星期内,注射部位会出现一个红色的小丘疹
- 2到3个星期后可能会发展为溃疡 (开放性疮) (直径通常小于1厘米),并持续数周至数月
- 溃疡愈合后,大部分婴儿手臂上的注射部位会形成一个扁平瘢痕。
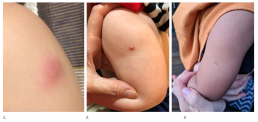
1. 丘疹
2. 溃疡
3. 瘢痕
罕见或较严重副作用包括:
- 腋窝淋巴结肿大(左臂下方的淋巴结肿胀)
- 溃疡持续超过数月
- 注射部分出现大块脓肿(脓液聚集)
- 注射部位形成瘢痕疙瘩
注意:如果你怀疑出现罕见或严重的副作用,我们强烈建议你向全科医生或者接种卡介苗疫苗的医疗诊所寻求医学咨询。如需获取免疫接种专家咨询或报告疫苗接种不良事件(AEFI),请联系SAEFVIC。。
疫苗接种后护理
在免疫接种后,注射部位必须保持干净、干燥。可以继续进行沐浴和游泳等正常活动,但结束后务必将接种部位擦干。
如果溃疡渗出浓液,可以用干燥纱布覆盖,以及使用酒精擦拭片进行清洁。接种部位不得直接涂抹药膏、乳霜或消毒剂。
了解更多信息,请参阅接种卡介苗疫苗后的注意事项 – 皇家儿童医院 (RCH) 父母手册。。
资源
昆士兰州卡介苗疫苗诊所
- 皇家儿童医院:卡介苗疫苗诊所
- Monash Health 免疫接种服务
- Offspring 儿童健康专科
- 家庭免疫接种及旅行专科(FITS)
- Mike Starr 副教授
- Craigieburn Specialist Consulting Suites
- Medical One - QV
- 儿童旅行医生
- 儿童私营医疗小组
- Wyndham 私营医疗中心
- 澳大利亚旅行诊所 - Caulfield
- Pinnacle Medical Centre – Williams Landing
- The Travel Doctor – TMVC at Sonic HealthPlus CBD clinic
- CBD Doctors Melbourne
其他
- MVEC:皮内免疫接种
- RCH 儿童健康信息: 结核病(TB)
- 澳大利亚免疫接种手册:结核病
- 皇家儿童医院儿童健康信息结核病卡介苗疫苗
- 接种卡介苗疫苗后的注意事项 – 皇家儿童医院父母手册
- 孩子接种卡介苗疫苗后的注意事项 – 莫纳什医院 (Monash Hospital) 父母手册
- Dhanawade, S. Kumbhar, S. Gore, A. and Patil, V. 婴儿接种卡介苗疫苗后的瘢痕形成与结核菌素转换: 前瞻性队列研究,Journal of Family Medicine and Primary Care 2015 Jul-Sep 4(3) 384-387
作者:Nigel Crawford(默多克儿童研究所SAEFVIC主任)和Rachael McGuire(默多克儿童研究所SAEFVIC研究护士)
审阅者:Rachael McGuire(MVEC教育护士协调员)
日期: 3 月 13, 2024
本章节内的材料将随着新信息和新疫苗的出现而进行更新。墨尔本疫苗教育中心(MVEC)职员定期审阅材料的准确性。
本站点的信息并非针对你个人健康或你家人个人健康的特定、专业的医疗建议。对于医疗方面的问题,包括有关免疫接种、药物治疗和其他治疗的决定,你务必咨询医疗保健专业人士。
伤寒
什么是流行性感冒?
Typhoid and paratyphoid fever are 引起的 bacterial infections with the Salmonella enterica subspecies Typhi 和 Paratyphi (A, B and C). Collectively, typhoid and paratyphoid fever 是 known as enteric fever. Typhoid fever presents more commonly than paratyphoid fever and is associated with higher rates of severe complications and poorer outcomes. T他 similarities between typhoid and paratyphoid fever make it difficult to distinguish between the two diseases without diagnostic testing.
Enteric fever is different to the gastroenteritis that can be caused by 其他 Salmonella 细菌.
流感症状
The incubation period of typhoid fever is usually 7 到 14 days but can range from 3 到 60 days. Typhoid and paratyphoid 发烧 often present with prolonged fever and fatigue, headache, splenomegaly (enlargement of the spleen), abdominal symptoms (pain, lack of appetite, constipation 或者 diarrhoea) 和 bacteraemia (bacteria in the bloodstream). A rash appearing as small pink clusters on the skin known as ‘rose spots’ can be seen in up to 30% of individuals with enteric fever. In severe cases, complications can include septic shock, gastrointestinal bleeding with perforation, altered conscious state. If left untreated, enteric fever can be fatal.
结核病是如何传播的?
Salmonella enterica is transmitted via the faecal–oral route and through ingestion of contaminated food and water sources. It is more common in developing countries with untreated drinking water and inadequate sanitation and food handling practices.
Approximately 10% of people infected with Salmonella enterica will excrete the bacteria for up to 3 months following acute infection. Approximately 1 in 20 infected individuals who do not receive treatment for typhoid fever will become an asymptomatic carrier of the disease.
流行病学
Although it is not prevalent in Australia, typhoid is a common disease in many parts of the world, especially Asia, southeast Asia and sub-Saharan Africa. In Australia, 100 to 200 returned travellers are diagnosed with typhoid every year
In 2019 it was estimated that 9 million cases of typhoid occur globally each year, resulting in 110,000 deaths. Children are disproportionately affected by infection.
预防措施
Prevention of typhoid 发烧 includes both vaccination and undertaking food and water precautions whilst travelling in developing countries where typhoid is endemic.
Food and water precautions
Travellers should maintain the following precautions to limit exposure to infections:
- undertake effective hand washing practices
- drink bottled or boiled water
- avoid ice ice unless it is made from safe water
- ensure food is properly cooked
- avoid raw milk and products made from raw milk
- wash fruits and vegetables carefully, particularly if they are eaten raw
- when possible, peel vegetables and fruits.
疫苗
There are 3 vaccines available in Australia for protection against typhoid fever:
| 年龄阶层 | Vaccine brand, antigen, dose and route | 初级课程 | 助推器 |
| ≥ 2 years | Typhim Vi (typhoid) 0.5 mL 我是 | 1剂 | after 3 years |
| ≥ 6 years | Vivotif (typhoid*) 1 capsule oral | 3 doses (day 1, 3 and 5) | after 3 years |
| 4 doses (day 1, 3, 5 and 7) | after 4 years | ||
| ≥ 16 years | Vivaxim (typhoid, hepatitis A) 1.0 mL 我是 | 2 doses (6 months apart) | typhoid only after 3 years (hepatitis A booster not required) |
Blue shading = live-attenuated vaccine
§ While Vivaxim is not registered for use in children aged under 16 years, some immunisation specialists and travel medicine practitioners administer Vivaxim to children aged 2–15 years. 参考 Lau C. et al The tolerability of a combined hepatitis A and typhoid vaccine in children aged 2-16 years: an observational study Journal of Travel Medicine 2016: 15, 23 (2) 了解更多信息。
* There is no specific vaccine for paratyphoid fever however there is some evidence to suggest that administration of the oral typhoid fever vaccine (Vivotif) can provide some cross–protection against paratyphoid fever.
Precautions and contraindications
People taking both the oral typhoid vaccine (Vivotif) and the oral cholera vaccine (Dukoral) should separate these 2 vaccines by 8 hours, due to the risk of components of the cholera vaccine impacting how the typhoid vaccine is absorbed.
Vivotif is live-attenuated vaccine and is therefore contraindicated in pregnant people and in individuals with immunocompromise.
People who are currently receiving antibiotics, sulfonamides or antimalarial prophylaxis should receive one of the injected typhoid vaccines (Typhim Vi or Vivaxim) instead of Vivotif. Alternatively, time the last dose of the oral vaccine at least 3 days before commencing antibiotics, sulfonamides or antimalarial prophylaxis.
疫苗副作用
Side effects from typhoid vaccination are usually mild and short lived.
注射部位反应 commonly occur in people who have received injected typhoid vaccines (Typhim Vi and Vivaxim). Abdominal pain, diarrhoea, nausea, vomiting and urticaria (itchy rash) commonly occur after vaccination with the oral typhoid vaccine (Vivotif).
资源
- Australian Immunisation Handbook: Typhoid fever
- The blue book: guidelines for the control of infectious diseases
- World Health Organization: Typhoid
作者: Rachael Purcell(RCH 免疫研究员)、Francesca Machingaifa(MVEC 教育护士协调员)和 Rachael McGuire(MVEC 教育护士协调员)
审核人: Rachael McGuire (MVEC Education Nurse Coordinator) and Katie Butler (MVEC Education Nurse Coordinator)
日期: November 2023
本章节内的材料将随着新信息和新疫苗的出现而进行更新。墨尔本疫苗教育中心(MVEC)职员定期审阅材料的准确性。
You should not consider the information on this site to be specific, professional medical advice for your personal health or for your family’s personal health. For medical concerns, including decisions about vaccinations, medications and other treatments, you should always consult a healthcare professional.
血栓形成伴血小板减少综合征 (TTS)
血栓形成伴血小板减少综合征 (TTS),也称为 疫苗诱导的血栓形成前免疫性血小板减少症 (VIPIT) 或 疫苗诱导的免疫性血栓性血小板减少症 (VITT),是一种罕见的综合症,在接受 腺病毒载体 新冠肺炎 疫苗,例如 Vaxzevria(阿斯利康)和强生/杨森 COVID-19 疫苗。
请注意:澳大利亚不再提供腺病毒载体 COVID-19 疫苗。以下信息仅供参考。
什么是语音合成?
该综合征的特征是血栓形成(血块)和血小板减少症(血小板计数低),通常在接种疫苗后 4-42 天内出现症状。
根据疾病控制中心 (CDC),TTS 根据血栓形成的位置和症状的严重程度分为 2 级。病例根据最近是否接触过肝素进一步分类。
第 1 层:
- 不常见的血栓形成部位(例如脑 - 脑静脉窦血栓形成 [CVST] 或肠道 - 例如内脏静脉,与肠缺血和手术相关,门静脉或其他罕见的静脉和动脉血栓形成)
- 也可能同时在更常见的位置发生血栓形成(例如深静脉血栓形成或肺栓塞)
- 血小板计数 < 150,000 每微升
- 阳性 (+) 抗 PF4 ELISA 结果支持,但不是诊断所必需的。
2级:
- 血栓形成的常见部位,如腿部或肺部(例如静脉血栓栓塞、深静脉血栓形成、肺栓塞)
- 血小板计数 < 150,000 每微升
- 需要阳性抗 PF4 ELISA 结果。
第 1 级往往与更严重的表现相关,并且比第 2 级具有更高的发病率和死亡率风险。有证据表明,第 1 级在较年轻的年龄组中更为常见。
腺病毒载体疫苗是如何触发 TTS 的?
TTS 是如何被触发的确切机制仍在调查中,但大多数病例与抗 PF4 抗体的发现有关。没有明确的诊断标记来表明谁有患这种综合征的风险。目前正在对此进行调查。
TTS 似乎类似于一种称为肝素诱导的血小板减少症 (HIT) 的自身免疫性疾病,即对肝素药物的免疫反应影响血小板功能,导致血栓形成(凝块)。
TTS的风险
据估计,Vaxzevria(阿斯利康)第 1 剂后发生 TTS 的风险约为每 100,000 人 2.6 人,其中 60 岁以下的人会经历更严重的后果。第 2 剂后发生 TTS 的风险要低得多。
接受腺病毒载体疫苗后发生其他凝血障碍的风险
目前没有证据表明腺病毒载体疫苗会增加发生其他独立血栓形成(例如导致深静脉血栓形成、肺栓塞、心肌梗塞、中风的其他凝血障碍)的总体风险超过一般人群的基线率。
TTS 不同于其他常见诊断的血栓形成,因为它是由对特定类型疫苗的免疫反应引发的,然后导致结合 两个都 血栓形成(凝块)和血小板减少症(低血小板计数)。
资源
- MJA:澳大利亚和新西兰疫苗诱导的免疫血栓形成和血小板减少症的诊断和管理方法
- 澳大利亚和新西兰血栓与止血协会 (THANZ) 多学科 VITT 医生指南
- HealthPathways 血栓形成伴血小板减少综合征 (TTS) 通路(需要登录)
- ATAGI 关于使用 COVID-19 疫苗阿斯利康的修订建议声明,2021 年 6 月 17 日
- ATAGI:ATAGI 和 THANZ 关于伴有血小板减少综合征 (TTS) 的血栓形成和 COVID-19 阿斯利康的使用的联合声明
- THANZ 血液学家咨询声明,2021 年 8 月 19 日:疑似疫苗诱导的免疫性血栓性血小板减少症 (VITT)
- 澳大利亚急诊医学院:接种 COVID-19 疫苗后出现血栓形成伴血小板减少综合征
- COVID-19 疫苗接种——免疫接种提供者关于 COVID-19 疫苗接种后血栓形成伴血小板减少综合征 (TTS) 的信息
- 关于阿斯利康 COVID-19 疫苗和血栓形成伴血小板减少综合征 (TTS) 的患者信息表
作者: Daryl Cheng(皇家儿童医院儿科医生)、Francesca Machingaifa(MVEC 教育护士协调员)、Davina Buntsma(MVEC 免疫研究员)和 Rachael McGuire(MVEC 教育护士协调员)
审核人: Linny Kimly Phuong(免疫顾问,SAEFVIC)、Rachael McGuire(MVEC 教育护士协调员)和 Hannah Morgan(流行病学家,SAEFVIC)
日期: 5 月 2, 2023
本章节内的材料将随着新信息和新疫苗的出现而进行更新。墨尔本疫苗教育中心(MVEC)职员定期审阅材料的准确性。
本站点的信息并非针对你个人健康或你家人个人健康的特定、专业的医疗建议。对于医疗方面的问题,包括有关免疫接种、药物治疗和其他治疗的决定,你务必咨询医疗保健专业人士。
Tetanus
什么是流行性感冒?
Tetanus 是 caused by infection with 细菌 Clostridium Tetani. 这 细菌 secrete a potent exotoxin that enter秒 the bloodstream, acting on the central nervous system 到 原因e muscle rigidity and painful spasms. Tetanus can be fatal when the muscles controlling respiration are affected.
流感症状
The incubation period of tetanus is 3 to 21 days. The most common time frame for presentation of tetanus is around 14 days after exposure. Although, it can present as early as 1 day or as long as several months after the exposure.
The initial symptom is muscle rigidity. This can affect all muscles in the body but may be more pronounced in those closest to the site of the injury. In some cases, symptoms may include hyperreflexia (hyperactive reflexes) resulting in back, neck or limb stiffness; trismus (lockjaw); or sardonic smile (dystonia, or involuntary muscle contractions, producing a fixed smile). As the disease progresses, painful muscle spasms occur, affecting any muscles simultaneously. When spasms and rigidity affect the respiratory or laryngeal muscles, sedation and/or prolonged ventilation in the intensive care setting is required. Examples of complications of tetanus include hypertension (high blood pressure), hypotension (low blood pressure), respiratory failure, cardiac arrythmias (irregular heartbeat), pneumonia, fractures, muscle rupture, deep vein thrombophlebitis, pulmonary emboli, decubitus ulcers and rhabdomyolysis. In severe cases, tetanus can be fatal.
结核病是如何传播的?
Tetanus spores are found in dirt, dust and animal faeces. They can survive in the environment for many years. Spores can be introduced into the body via a wound where the bacteria can grow and cause infection. Spores can survive in a wound for as long as 3 months before becoming active.
Tetanus can occur following a significant wound or after trivial or even unnoticed wounds. Examples of wounds that are considered tetanus-prone include:
- 动物或人的咬伤
- 深部穿透伤
- minor lacerations, for example, from cat scratches, rose thorns, glass or other foreign bodies (e.g. splinters)
- contusions or burns
- compound (open) fractures
- 被户外设备割伤或割伤
- tooth reimplantation post avulsion (knocked out tooth)
- 静脉注射毒品的场所。
Tetanus cannot be passed directly from person to person.
流行病学
The incidence of tetanus is rare in Australia. Since 2001, there have been fewer than 8 cases reported each year, with a total of 84 cases since 2000. The case fatality rate in Australia is about 2%. Globally, tetanus is fatal in approximately 11% of reported cases.
Tetanus can affect people of any age. However infections in Australia are more commonly seen in older adults who have never been vaccinated or were vaccinated more than 10 years ago.
In countries with low rates of vaccination, Maternal and Neonatal Tetanus (MNT) remains a common life-threatening consequence of unhygienic deliveries and umbilical cord care practices. Mortality rates associated with MNT are extremely high, especially when appropriate medical care is not available, as is often the case.
预防措施
Vaccination is the most effective way to prevent tetanus. Vaccines target the tetanus toxin (toxoid) and, in Australia, are available only in combination with diphtheria. Vaccines may also include other antigens, such as pertussis, inactivated poliovirus, hepatitis B and haemophilus influenzae type B.
Table: Which tetanus-toxoid containing vaccine to use by age of patient
| 年龄阶层 | Vaccine brand, antigen, dose and route | |||||
| Infanrix Hexa/Vaxelis (DTpa, hep B, Hib, polio) 0.5 mL 我是 | Infanrix/Tripacel (DTPa) 0.5 mL 我是 | Infanrix-IPV/Quadracel (DTPa, polio) 0.5 mL 我是 | Boostrix/Adacel (dTpa) 0.5 mL 我是 | Boostrix IPV/Adacel Polio (dTpa, polio) 0.5 mL 我是 | ADT (dT) 0.5 mL 我是 | |
| 6 weeks to < 10 years | ✓ | ✓ | ✓ | |||
| ≥ 10 years | * | ✓ | ✓ | ✓ |
Tick = recommended for use in this age group
Grey shading = not routinely recommended for use in this age group
* ATAGI recommends the use of Infanrix hexa and Vaxelis in children aged < 10 years, however the Royal Children’s Hospital (RCH) preferentially uses them up to < 18 years in instances where multiple vaccines are required (eg. catch up, post chemotherapy/post HSCT).
初级课程
As per the National Immunisation Program (NIP), a primary course of tetanus vaccination is given at 6 weeks, 4 months, and 6 months of age (Infanrix hexa/Vaxelis).
Boosters
Booster doses are scheduled to be administered at:
- 18 months (Infanrix/Tripacel)
- 4 years (Infanrix-IPV/Quadracel)
- 12 to 13 years of age/year 7 high school program (Boostrix)
Regular booster doses every 10 years are no longer routinely recommended. However, women who receive the recommended pertussis vaccine during every 怀孕 will also receive a booster of tetanus (and diphtheria). Adults aged ≥ 50 years who have not received a dose of tetanus-containing vaccine in the last 10 years should consider a booster dose (unfunded).
Those who have a tetanus-prone wound should also receive a booster if they have not received a dose of tetanus-containing vaccine in the last 10 years (see Tetanus-prone wounds below).
Catch up
Any person with an incomplete tetanus immunisation history should be offered catch up. Refer to MVEC: Catch up immunisation for specific guidance.
Tetanus-prone wounds
The correct management of a tetanus-prone wound is vital for the prevention of tetanus infection.
Initial treatment involves cleaning and disinfecting the wound. Medical review by a GP or emergency department is recommended.
Reviewing a person’s immunisation history will inform tetanus-prevention management, which may include vaccination and/or the administration of immunoglobulin. Immunoglobulin provides short-term protection against tetanus. Vaccines provide longer and ongoing protection against the development of disease.
Regardless of the nature of the wound, all unimmunised individuals, partially immunised individuals(those who have received less than 3 doses of a tetanus-containing vaccine) and 免疫功能低下 individuals are at the greatest risk of contracting tetanus.
Groups who are often assumed to be up to date, but may lack optimal vaccine protection, include:
- those aged 9-13岁之间, as they are 5 + years post their 4-year-old vaccine and may not have yet received their Year 7 booster
- 这 elderly population, due to waning immunity and time passed since last booster.
Table: Guide to tetanus-prevention management
| Vaccine history of tetanus-containing vaccine | Time since last dose | Clean, minor wounds | Other wounds | ||
| Vaccination ¥ | Immunoglobulin | Vaccination ¥ | Immunoglobulin | ||
| ≥ 3 doses | < 5 年 | * | |||
| 5–10 years | ✓ | * | |||
| > 10 years | ✓ | ✓ | * | ||
| < 3 doses / uncertain | Any time / uncertain | ✓^ | ✓^ | ✓ |
Tick = required
Shaded boxes = not required
¥ Using age-appropriate tetanus-containing vaccine (see above Table: Which tetanus-toxoid containing vaccine to use by age of patient)
*administration of immunoglobulin is recommended when the patient has humoral immune deficiency or HIV (regardless of CD4+ count)
^ where there is no documented history of a completed 3-dose primary course of tetanus vaccination patients should receive all missing doses AND tetanus immunoglobulin.
疫苗副作用
Injection site reaction (ISR) is a common side effect after receiving a tetanus-toxoid vaccine. Uncommon side effects include headache, lethargy, irritability, body aches and fever. These side effects are usually self-limiting and resolve within 48 hours.
作者: Lynne Addlem(免疫护士,皇家儿童医院)和 Rachael McGuire(教育护士协调员)
审核人: Katie Butler (MVEC Education Nurse Coordinator) and Rachael McGuire (MVEC Education Nurse Coordinator)
日期: November 2023
本节内的材料将随着新信息的出现而进行更新。MVEC职员定期审阅材料的准确性.
You should not consider the information on this site to be specific, professional medical advice for your personal health or for your family’s personal health. For medical concerns, including decisions about vaccinations, medications and other treatments, you should always consult a healthcare professional.
旅行药
旅行医学侧重于疾病预防和伤害风险最小化,并根据旅行人员的个人情况(例如旅行的地点和目的、一年中的持续时间和时间)以及任何潜在的医疗状况或其他风险因素提供建议。
从哪里获得旅行建议
全科医生和旅行医学诊所可以提供预防保健建议并提供疫苗接种。还有专门研究传染病或免疫接种的儿科医生可以为儿童(及其家人)提供建议。还可以访问许多出色的网站,以获取特定国家/地区的更新和有关新发感染的信息 [请参阅下面的参考资料]。
何时寻求建议
对于特定的旅行前建议,最好在出发前至少 4-6 周咨询医疗保健专业人员,这样可以在到达旅行目的地之前有时间在接种任何推荐的疫苗后产生免疫力。根据推荐的疫苗,在一个人被认为完全受到保护之前,可能会指示一段时间的疫苗接种过程。
由于大多数旅行专家需要 GP 转介并且可能需要等待预约时间,因此将这一点纳入旅行计划时间表非常重要。
疫苗
一些常规疫苗可以比预定时间提前接种或作为旅行目的的额外剂量接种。这方面的例子包括:
- 麻疹死亡率 (麻疹、腮腺炎和风疹)疫苗:如果前往麻疹流行地区旅行,可以在 6-11 个月之间接种一剂额外的、受资助的剂量
- 脑膜炎球菌 疫苗:
- MenACWY (Nimenrix) 疫苗可以从 6 周龄开始接种,以提供更早的保护(NIP 规定在 12 个月大和中学 10 年级时接种)
- B 型脑膜炎球菌 (Bexsero) 疫苗也可以从 6 周龄开始接种(国家免疫计划 (NIP) 不资助所有人,但可以为不符合资助剂量的人私人购买)
- 流行性感冒 疫苗:根据一年中的时间和旅行目的地,接种流感疫苗可能是明智的
- 新冠肺炎 疫苗:由于不断出现 COVID-19 疾病毒株,重要的是要确保完成 COVID-19 疫苗接种的初级疗程以及根据当前建议推荐的任何加强剂。
其他与旅行相关的疫苗,取决于您的位置和旅行时间,可能包括:
其他注意事项
其他旅行准备可能包括:
- 考虑到预防疟疾的必要性(药物预防疟疾)
- 预防蚊媒疾病的措施,例如穿长袖衣服、蚊帐和含有避蚊胺的驱虫剂
- 食品和水安全。
免疫力低下和怀孕的旅客
个人是 免疫功能低下 由于身体状况或特定疗法,鼓励尽早寻求旅行建议,以在旅行前最大限度地预防疫苗可预防的疾病。
同样,计划怀孕或正在怀孕的妇女 孕, 应尽早寻求旅行建议,以确保为母亲和未出生的婴儿提供最佳保护。计划怀孕且旅行可能性很高的女性应考虑在怀孕前接种疫苗,并注意减毒活疫苗在怀孕期间是禁忌的。
探亲访友 (VFR)
VFR 旅行是国际旅行最常见的原因之一。 VFR 旅行者是指从他们居住的高收入国家前往他们的低收入出生国家探望朋友或亲戚的移民。 VFR 旅行前的旅行咨询应考虑个人是否接种过常规 NIP 疫苗或有疫苗可预防疾病的病史,以及是否接种了适合他们前往的国家/地区的疫苗。该人群中某些与旅行相关的感染率较高,因此采取适当的预防措施(例如接种疫苗)以及考虑食品和水安全对于确保最佳保护非常重要。
资源
MVEC 旅游相关资源
其他资源
作者: Nigel Crawford(默多克儿童研究所 SAEFVIC 主任)和 Rachael McGuire(默多克儿童研究所 SAEFVIC 研究护士)
审核人: Rachael Purcell(RCH 免疫研究员)、Francesca Machingaifa(MVEC 教育护士协调员)和 Rachael McGuire(MVEC 教育护士协调员)
日期: June 8 2023
本章节内的材料将随着新信息和新疫苗的出现而进行更新。墨尔本疫苗教育中心(MVEC)职员定期审阅材料的准确性。
本站点的信息并非是针对您或您家人个人健康的特定、专业的医疗建议。对于医疗方面的问题,包括有关免疫接种、药物治疗和其他治疗的决定,请务必咨询医疗保健专业人士。